Last year, my husband and I took a 16-day road trip from Kentucky through Massachusetts to Maine. On our first morning in Boston, we exited the Park Street Station en route to Boston Common but instead of being greeted by the aroma of molasses, we were hit full-on with a pungent repulsive odor. "That's skunk weed," my husband chuckled as we stepped right into the middle of The Boston Freedom Rally, a celebration of all things cannabis.
As we boarded a hop-on-hop-off bus, we learned that this was the one week of the year that the city skips testing tour bus drivers for tetrahydrocannabinol (THC), "because we all test positive," the driver quipped. As our open-air bus circled the Common, a crowd of pot enthusiasts displayed signs in support of relaxed regulation for public consumption.
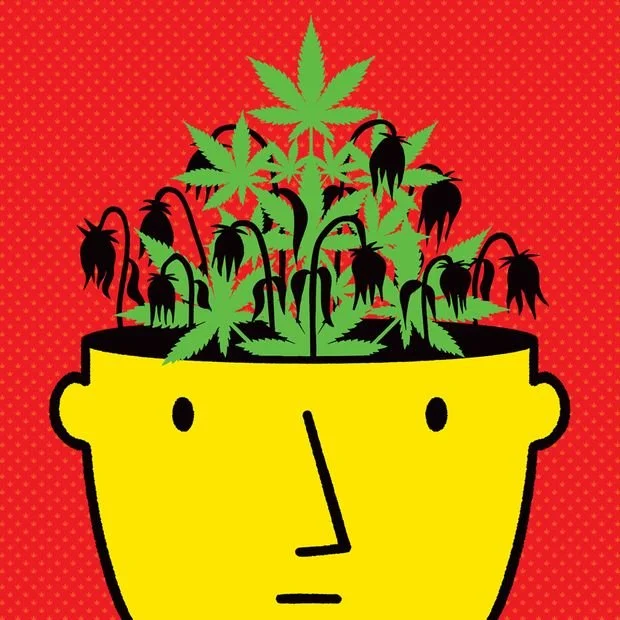
The 34-year-old Boston Freedom Rally is a sign that US culture has transformed forever. Mary Jane is no friend of emergency physicians nor of staff on hospital wards and offices. Healthcare workers should brace for the true impact of THC as its adoption by all ages rises.
Toking Boomers and Millennials
Researchers at University of California, San Diego looked at cannabis-related emergency department visits from all acute-care hospitals in the state from 2005 to 2019 and found an 1808% increase in patients aged 65 or older (that is not a typo) who were there for complications from cannabis use.
The lead author said in an interview that, "Older patients taking marijuana or related products may have dizziness and falls, heart palpitations, panic attacks, confusion, anxiety or worsening of underlying lung diseases, such as asthma or [chronic obstructive pulmonary disease]."
A recent study from Canada suggests that commercialization has been associated with an increase in related hospitalizations, including cannabis-induced psychosis.
According to a National Study of Drug Use and Health, marijuana use in young adults reached an all-time high (pun intended) in 2021. Nearly 10% of eighth graders and 20% of 10th graders reported using marijuana this past year.
The full downside of any drug legal or illegal is largely unknown until it infiltrates the mainstream market, but these are the typical cases* we see:
Let's start with the demotivated high school honors student who dropped out of college to work at the local cinema. He stumbled and broke his clavicle outside a bar at 2 AM, but wasn't sure if he passed out so a cardiology consult was requested to "rule out" arrhythmia associated with syncope. He related that his plan to become a railway conductor had been upended because he knew he would be drug tested and just couldn't give up pot. After a normal cardiac exam, ECG, labs, a Holter, and an echocardiogram were also requested and normal at a significant cost.
Cannabinoid Hyperemesis Syndrome
One of my Midwest colleagues related her encounter with two middle-aged pot users with ventricular tachycardia (VT). These episodes coincided with potassium levels < 3.0 mEq/L in the setting of repetitive vomiting. The QTc interval didn't normalize despite a corrected potassium level in one patient. They were both informed that they should never smoke pot because vomiting would predictably drop their K+ levels again and prolong their QTc intervals. Then began "the circular argument" as my friend described it. The patient claims, "I smoke pot to relieve my nausea," to which she explains that "In many folks, pot use induces nausea." Of course, the classic reply is, "Not me." Predictably one of these stoners soon returned with more VT, more puking, and more hypokalemia. "Consider yourself 'allergic' to pot smoke," my friend advised, but, "Was met with no meaningful hint of understanding or hope for transformative change," she told me.
I've seen cannabinoid hyperemesis syndrome several times in the past few years. It occurs in daily to weekly pot users. Very rarely, it can cause cerebral edema, but it is also associated with seizures and dehydration that can lead to hypovolemic shock and kidney failure.
Heart and Brain Harm
Then there are the young patients who for various reasons have developed congestive heart failure. Unfortunately, some are repetitively tox screen positive with varying trifectas of methamphetamine (meth), cocaine, and THC; opiates, meth, and THC; alcohol, meth, and THC; or heroin, meth, and THC. THC, the ever present and essential third leg of the stool of stupor. These unfortunate patients often need heart failure medications that they can't afford or won't take because illicit drug use is expensive and dulls their ability to prioritize their health. Some desperately need a heart transplant but the necessary negative drug screen is a pipe dream.
And it's not just the heart that is affected. There are data linking cannabis use to a higher risk for both ischemic and hemorrhagic stroke. A retrospective study published in Stroke of more than 1000 people diagnosed with an aneurysmal subarachnoid hemorrhage found that more than half of the 46 who tested positive for THC at admission developed delayed cerebral ischemia (DCI), which increases the risk for disability or early death. This was after adjusting for several patient characteristics as well as recent exposure to other illicit substances: cocaine, meth, and tobacco use were not associated with DCI.
Natural My…
I'm certain my anti-cannabis stance will strike a nerve with those who love their recreational THC and push for its legal sale, after all, "It's perfectly natural." But I counter with the fact that tornadoes, earthquakes, cyanide, and appendicitis are all natural but certainly not optimal. And what we are seeing in the vascular specialties is completely unnatural. We are treating a different mix of complications than before pot was readily accessible across several states.
Our most effective action is to educate our patients. We should encourage those who don't currently smoke cannabis to never start and those who do to quit. People who require marijuana for improved quality of life for terminal care or true (not supposed) disorders that mainstream medicine fails should be approached with empathy and caution.
A good rule of thumb is to never breathe anything you can see. Never put anything in your body that comes off the street: Drug dealers who sell cannabis cut with fentanyl will be ecstatic to take someone's money then merely keep scrolling when their obituary comes up.
Let's try to reverse the rise of vascular complications, orthopedic injuries, and vomiting across America. We can start by encouraging our patients to avoid "skunk weed" and get back to the sweet smells of nature in our cities and parks.